
High-Value, Simplified Health Care Options for Employers
How one population health management firm’s advanced analytics paved the way.

It’s no surprise that since the pandemic, employees’ health and wellness have taken center stage. More than half (56%) of organizations have increased spending on physical and mental health support for employees, according to the Risk Outlook 2022 report from International SOS.* Not only that, but employers want to provide employees with a more customized insurance benefits package for both employee retention and workplace satisfaction. If they can impact their own costs for employer-sponsored health care, even better. The bottom line is they’re looking for alternatives to payer models that take control away from the company and place it in the hands of a third-party payer.
The people at population health management firm Populytics, Inc., knew the time was right for a more satisfying solution. Especially considering the company had spent years building the infrastructure necessary to navigate and succeed in an environment inching its way to value-based care versus fee-for-service, fully understanding that value-based care was the certain eventuality. Upon establishing a solid foundation, Populytics is able to offer a comprehensive program for self-insured employers that strips away the layers and consolidates health care management. Populytics Health Management Solutions (PHMS) gets straight to the heart of what employees want: high-value, simplified health care.
Data and Analytics are the Foundation
In today’s world, the demand for value-based medical care has made predictive and preventive measures essential. Only data makes these measures possible and only analytics makes them applicable to the care of patients and the population. It means, instead of simply addressing patients’ symptoms, practitioners can identify people at risk of developing chronic illnesses and treat them before conditions become serious. This translates to more informed care as well as efficiencies that come from mitigating long-term issues and expensive hospitalizations.
If hospitalization of patients is necessary, data analytics make it possible to predict what might come next, from health deterioration and risk of infection to readmission. This provides an added benefit of handling problems with more efficiency and less risk.
This predictive insight gives Populytics the edge in terms of optimizing the quality and value of the health care delivered, which is the cornerstone of value-based care and of PHMS. As one expert noted regarding this general ability, ”When you can do this modeling, you can tug on different threads and see what the impact will be, clinically, value-based-care wise, and financially, to solve real problems. Data is the key to allowing organizations to safely move forward with different initiatives – and, in doing so, improve patient outcomes and move the field, as a whole, forward.”**
The Advantage of Integration
Another important element of a successful alternative to traditional employer-sponsored health care is being able to circumvent the complexities. Direct-to-Employer (D2E) health care does that. However, many health care providers in D2E arrangements – usually large health systems – often don’t have the necessary skills and processes to cover all the bases without involving a third party. PHMS differs in that, through alignment with one of eastern Pennsylvania’s largest health systems and its affiliated physician/APC organization, it has all the knowledge, competencies, and talents to offer a direct solution that is truly comprehensive.
One important competency is a highly developed care coordination function, where the primary care practice enables information sharing among all the providers involved with a patient's care. In the PHMS model, providers are paid for maintaining and improving the health of their patient panels. Population health initiatives’ clinical and financial results strongly rely on preventing illness progression while continuing to care for patients when illness strikes, therefore, the approach is built upon an integrated effort.
“An expanded care team has become more critical than ever before,” says Jonathan Burke, DO, CHCQM, Medical Director, Clinical Services at Populytics. “Physicians can’t do it alone and should not be expected to.” The “team” at work in PHMS includes physicians, Advanced Practice Clinicians (APCs), social workers, nurse case managers, and pharmacists who are available to support a patient’s plan of care.
A History of Health Plan Management
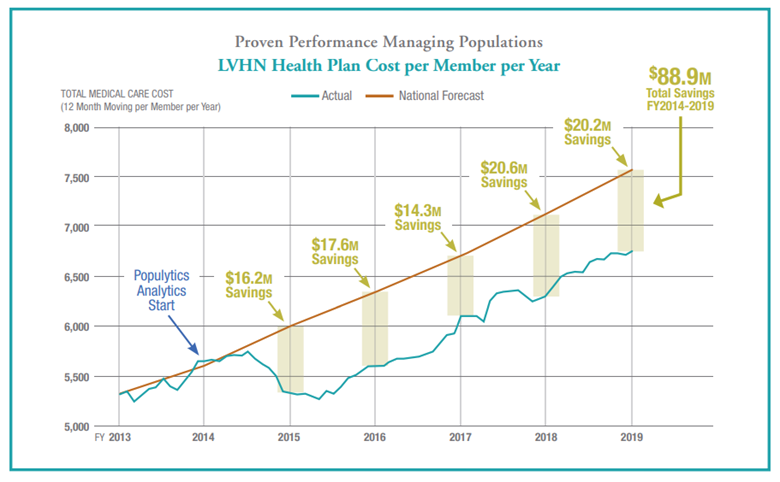
Experience in health plan management is an essential aspect of building the foundation to a new concept such as direct-to-employer health care. Populytics as a company emerged from a tradition of third-party administration, health plan design, and claims processing, giving its staff the knowledge necessary for competent execution of a D2E plan. Successful management of the self-funded health plan for Lehigh Valley Health Network – which comprises more than 26,000 members – realized $90 million in savings over the first five years. (See the graph below.)
When experience, highly developed care coordination, advanced health care analytics, and physician engagement come together in a direct-to-employer solution, the results for employers are tangible. You have more control over health care expenditures, more control over health plan design, and more potential economies from less involvement by major insurers. Those benefits, inherent in PHMS, may be just the right fit for employers who are looking for a self-insured solution to the rising cost of company-sponsored health care coverage.
* https://2022.risk-outlook.com/p/1
**https://www.healthcareitnews.com/news/making-smarter-decisions-data-analytics
Gain control over employee health care by going directly to the source


